Despite widespread discussion of measurement‑based care in behavioral health, clear, organization‑level evidence of patient improvement remains rare. Many organizations describe processes, tools, or infrastructure, but few publicly report standardized, validated outcomes showing that patients actually get better.
At Array Behavioral Care, we believe transparency around outcomes is not optional—it is foundational to accountable, high‑quality care. As a national, fully virtual behavioral health provider, delivering care entirely through telehealth, we are committed to reporting rigorous, comparable clinical outcomes that partners can trust.
This brief preview highlights early findings from our upcoming outcomes white paper, focused on our virtual outpatient service line. It offers a data‑driven snapshot of how patients with depression improve over time when treated in a real‑world, outpatient telehealth setting.
Sustained Depression Symptom Improvement Over Six Months
These results reflect outcomes for patients who completed an initial intake in the first half of 2025, with follow‑up measured six months post‑intake. This approach allows us to assess durable clinical change, rather than short‑term fluctuations.
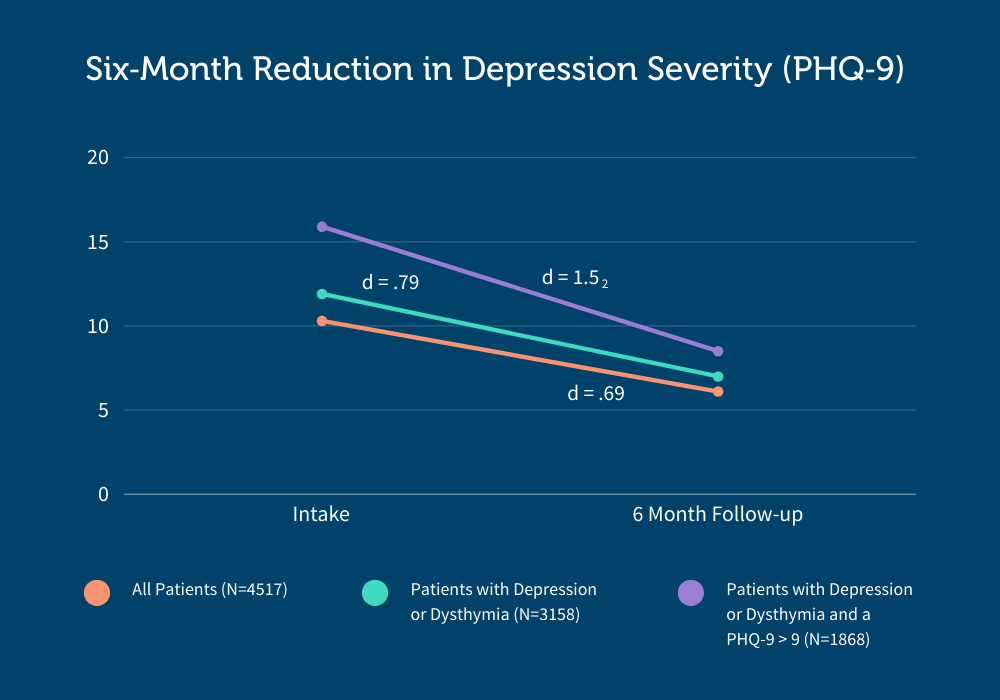
Across patients receiving therapy, psychiatry, or both services, depressive symptoms declined substantially and were maintained through six months of follow‑up. Improvements were observed across multiple patient subgroups and service configurations.
To ensure interpretability, outcomes are reported using standardized effect sizes (Cohen’s d)—a widely accepted metric in clinical research that conveys not just whether change occurred, but how meaningful that change was.
For patients with moderate or greater depression at intake (PHQ‑9 > 9), symptom reductions were large to very large in magnitude, with effect sizes exceeding what is typically reported in real‑world outpatient settings.
How Our Outcomes Compare to Industry Benchmarks
To understand the clinical significance of these results, we compared Array’s outcomes with published benchmarks from large, real‑world outpatient depression care settings, including integrated health systems and integrated care programs.
Using consistent, validated definitions of response and remission allows for meaningful, apples‑to‑apples comparison across care models. When evaluated this way, Array’s outcomes meet or exceed those reported in peer‑reviewed studies of real‑world outpatient depression care. These results highlight what is possible when outpatient mental health care is intentionally designed using measurement‑based practices, standardized care pathways, and longitudinal follow‑up.
Patients with Depression or Dysthymia and Elevated Baseline Symptoms (PHQ‑9 greater than 9)
| Metric | Description | Array Outcome | Large Integrated Health System Outcome1 | Large Integrated Care Program Outcome2 |
|---|---|---|---|---|
| Remission | % with Score less than 5 at Last Follow-Up | 27% | 22% | 16% |
| Response | % with Score less than 10 at Last Follow-Up | 56.7% | 46% | 47% |
Across both remission and response, Array’s outcomes compare favorably with established benchmarks from real‑world depression care.
Taken together, these outcomes exceed what is typically reported in the published literature for real‑world outpatient depression care. Seeing results of this magnitude, sustained over six months, reflects the rigor, consistency, and clinical seriousness of Array’s care model. These findings reinforce our commitment to delivering care that meaningfully improves patients’ lives, not just process metrics.
References
- Coley, R. Y., Boggs, J. M., Beck, A., Hartzler, A. L., & Simon, G. E. (2020). Defining Success in Measurement‑Based Care for Depression: A Comparison of Common Metrics. Psychiatric Services, 71(4), 312–318.
- Jeffrey, J., Klomhaus, A., Aralis, H., et al. (2021). Factors associated with response and remission from depression at 6 months of treatment in an integrated care program. BMC Health Services Research, 21(1), 703.
Why This Matters
Outcomes of this magnitude—sustained over six months and measured using standardized clinical metrics—highlight the impact of care design, not care setting. When evidence‑based treatment, measurement‑based care, and structured pathways are implemented consistently, outpatient mental health care can deliver meaningful, lasting improvement at scale.
Just as importantly, reporting outcomes using standardized metrics allows partners to make apples‑to‑apples comparisons across programs and providers, moving the field beyond process claims toward true accountability.
What’s Next
This preview represents an early look at a much larger outcomes dataset. In the full white paper and upcoming publications, we will explore:
- Outcomes across additional diagnoses, including anxiety
- Differences by service mix (therapy, psychiatry, and combined care)
- Engagement, access, and patient experience metrics
- Clinical outcomes across acuity levels and populations
We hope this work encourages the behavioral health field to raise the bar on transparency and to focus on what matters most: whether people are actually getting better.
Coming Soon
Full outcomes, methods, and comparative analyses will be released in the forthcoming Array Behavioral Care outcomes white paper.
Be the first to receive the full outcomes whitepaper, including detailed methods, expanded results, and additional analyses.
