Established in 2006, the Whiteside County Community Health Clinic (WCCHC) in Rock Falls, Illinois, was created to answer a long-standing need for medical, dental and behavioral healthcare among county residents. In 2018 alone, the clinic provided services to over 13,000 patients during more than 50,000 visits. As a federally qualified health center (FQHC), the clinic provides services to patients on a sliding fee scale, ensuring residents can access care regardless of their ability to pay.
By 2018, WCCHC’s behavioral healthcare team had grown to 11 therapists and one part-time psychiatrist, who served an ever-growing number of patients in need of specialized mental healthcare and medication management. Despite this high demand, the clinic’s psychiatrist stopped seeing patients, creating a pressing need to find a replacement. In-house staff were not equipped to handle complex patient needs, so the clinic was forced to refer patients elsewhere, losing thousands of dollars in patient billings to external providers.
WCCHC needed a clinician to fill a unique set of needs: someone young and energetic who could handle complex cases, engage easily with patients and staff, onboard quickly, and have the flexibility to adjust their hours as needed over time. After local recruitment efforts proved challenging, the clinic looked for an experienced telepsychiatry partner to help fill this tall order
WCCHC ultimately chose Array Behavioral Care, a leading provider of integrated telepsychiatry services. Array's broad clinician network gave WCCHC access to a large pool of highly specialized quality clinicians. In addition, the ability to provide comprehensive support services, including deployment, IT, reimbursement and regulatory insight, made Array an ideal partner.
Array identified a psychiatrist who met all of WCCHC’s criteria, helping the clinic launch its telepsych program in just two months. Once on board, the teleclinician quickly embedded herself in operations, working closely with the on-site care team to adapt to workflows and develop care plans for patients. She was an instant hit with patients and staff alike and has become a seamless part of clinic operations.
To maximize telepsych utilization, WCCHC focused on ways to reduce the patient no-show rate and improve access to care. Clinic staff identified potential barriers to patients in need and sought to address them in a variety of ways using funding from federal grants. If transportation is preventing patients from getting to appointments, the clinic offers them gas cards to pay for fuel. If affordability is preventing patients from taking needed medications, the clinic offers them pharmacy gift cards. To accommodate patient requests for same-day and soonest-available appointments, the clinic maintains a waitlist and contacts patients as time slots become available.
WCCHC uses ArrayConnect to ensure the best possible video quality for patient sessions, and has also used the platform to collect feedback through patient surveys to make sure it’s meeting patient needs. In addition to IT support, Array helps oversee all related program needs, including clinician management, compliance support and reimbursement.
Since implementing its telepsychiatry program with Array, WCCHC has been able to meet the behavioral healthcare needs of its community more efficiently and effectively. Key benefits include:
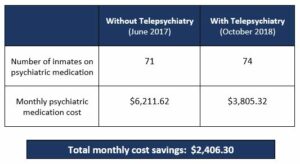
Prior to starting telepsychiatry, Mifflin County Correctional facility faced high cost of psychiatric medication for inmates.
Within the first month of partnering with Array for telepsychiatry services, Mifflin County Correctional Facility lowered their psychiatric medication cost by $1,503.42. A comparison of monthly pharmacy costs pre- and post-initiation of telepsychiatry services further demonstrates the cost savings they realized with telepsychiatry and proper formulary adherence.
Mifflin Country Correctional Facility found the transition to telepsychiatry seamless and easy and credits Array for the continued success of their program. They cite Array's ongoing support and commitment to quality care, timely communication and provider matching as reasons for their success. They consider their telepsychiatry providers a great fit for their organization and appreciate that these providers have been flexible, responsive, and willing to testify – even at the last minute – for mental health hearings.
Telepsychiatry offers access to corrections-specific psychiatrists who understand the nuances of treating incarcerated individuals while maintaining adherence to a strict formulary which leads to significant savings on psychiatry medication.
The yoga sessions and health bingo nights you’ll find at an Oak Street Health center are the first sign that it’s not your typical healthcare facility. With a mission to “rebuild healthcare as it should be,” the network of primary care practices for Medicare patients focuses on caring for the whole person to keep patients healthy and promote their well-being.
For Oak Street Health, providing quality mental health services is key to its integrated care approach. Founded in Chicago in 2013, the organization now serves 40,000 Medicare patients across five states – one-third of whom experience a mental health condition. As a value-based care provider, Oak Street is also incentivized to keep total healthcare costs down for each patient by focusing on preventive care.
By delivering behavioral health services directly to patients, Oak Street sought to help them get the care they need, improve their overall health and reduce expensive – and sometimes avoidable – hospital admissions. As a rapidly expanding network based in underserved neighborhoods, Oak Street also needed a way to access high-quality mental health providers and scale its services quickly. Recognizing that telepsychiatry aligned with its mission to provide efficient, effective whole-person care, Oak Street launched its mental health service program with Regroup in 2016.
Through its leading integrated telepsychiatry services, Regroup empowers healthcare organizations to bring quality mental health care services directly to patients, regardless of where they live. Since beginning their partnership, Regroup has provided Oak Street with the clinicians, tools and flexible support it needs to make the program a success.
As Oak Street works to optimize mental health care delivery and patient utilization, Regroup’s services have evolved alongside the organization’s needs. Over the past two years, Oak Street has added on-site behavioral health specialists at its locations to support patient engagement, and Regroup’s clinicians work closely with in-person staff to develop individualized care plans for each patient. Regroup has also helped to establish effective telepsychiatry technology, with both Regroup clinicians and other Oak Street telepsychiatrists relying on the RegroupConnect™ videoconferencing platform for patient sessions.
The two telepsychiatrists currently serving Oak Street have established ongoing relationships with their own patient populations over time, ensuring continuity of care and regular follow-up, explains Katherine Suberlak, Oak Street’s VP of population health. The clinicians are experienced at working within primary care settings, are flexible in accommodating scheduling changes when needed, and are accessible to on-site primary care and behavioral health teams to ensure a collaborative approach to care. That hands-on support extends to the rest of the management team, Suberlak says, with Regroup working closely with Oak Street to assess the quality of care and workflow and to ensure continuous quality improvement in service delivery.
Since implementing its telepsychiatry program with Regroup, Oak Street has been meeting its patients’ significant mental health needs with an effective, scalable program. Key benefits include:
Increasing patient utilization. Oak Street’s unique integrated approach is encouraging more patients to take advantage of behavioral health services and reducing no-show “A Regroup telepsychiatrist and the on-site behavioral health specialist now see certain high-risk patients together, helping to improve care collaboration and patient engagement, and ensuring follow-through on the psychiatrist’s recommendations,” population health specialist Lydia Vazquez says.
A financially stable program. As a value-based care provider, Oak Street is able to provide its Medicare patients with transportation to clinic Offering mental health services virtually on-site helps Oak Street ensure more patients are getting the care they need, resulting in healthier patients and fewer expensive acute care episodes.
A best practice-focused With support from Regroup, Oak Street has uncovered what works for its clinics and is applying those practices as it continues to expand. That includes establishing efficient patient check-in procedures, using e-prescribing for medications, using an electronic health record that different clinicians can access to provide collaborative care, and having a consistent clinician at each site to promote continuity of care.
“What we appreciate most about Regroup is their partnership and ongoing collaboration. As we work to optimize our delivery of mental health care services, they are always willing to work with us to find new ways to serve Oak Street and our patients effectively.”
Katherine Suberlak, VP of Population Health, Oak Street Health
Problem: 125/150 inmates on medication before telepsychiatry
Outcomes: With proper pharamcology via telepsychiatry, this number was reduced to only 30 inmates on medication.
Conclusions: Proper pharamcology with appropriate care and medication solves problems of over or under treating inmates. It also reduces number of inmates who try to “work the system” and saves tax payer dollars.
Problem: High cost of medication for inmates before telepsychiatry
Outcomes: With telepsychiatry and proper formulary adherence they were able to reduce pharmacy costs by almost 2/3 per month and nearly $480,000 annually.
Conclusions: Having access via telepsychiatry to psychiatric prescribers who are well-versed in correctional psychiatry and pharmaceutical options leads to major savings on psychiatric medication.
Telepsychiatry has proven efficient and effective, as is evident by case studies of Array's customers and other clinical research data.
Prisoners with psychiatric emergencies are treated expeditiously reducing liability to the arresting agency. More importantly police officers are spending less time at health care facilities guarding prisoners and are available to protect and serve civilians.
Telepsychiatry also represents access to corrections- specific psychiatrists who are sensitive to the nuances of treating offenders while maintaining adherence to a strict formulary.
Direct Cost Benefits of Telepsychiatry for Jails:
- Lower transportation cost
- Reduce custody & overtime expense
- Reduce offsite (ED) expense
- Lower call obligation expense
- Improve formulary adherence
- Provider suicide watch release
Indirect Cost Benefits of Telepsychiatry in Jails:
- Reduce flight risk
- Improve public safety
- Improve relationships with community providers
- Provide proper inmate care and safety
By: Chief Raymond J. Hayducka, MS, CPM, South Brunswick Police Department
The New Jersey Police Chief
Published: July/August 2009
Most law enforcement agencies throughout New Jersey and the United States are feeling the effects of the economy. This has compelled agencies to reduce costs and do more with less. Through a shared service program law enforcement officials in Middlesex County were able to find a cost effective solution to a problem that has impacted most agencies at one time.
Problem: Police Officers in Middlesex County are required to transport and guard prisoners that are experiencing a psychiatric emergency or threatening suicide prior to being lodged in the county jail on criminal charges.
The prisoner would have to be medically cleared because the correctional facility is not set up to care for prisoners with psychiatric emergencies. Quite often police officers would end up guarding these prisoners at local hospitals for long periods of time due to mental health professionals being unavailable during off hours and weekends to diagnose them.
During a monthly meeting of the Middlesex County Association of Chiefs of Police the issue of guarding prisoners with psychiatric emergencies was discussed.
Middlesex Borough Chief James Benson brought forth the problem after a particularly frustrating experience his agency recently dealt with.
Middlesex Borough Officers were required to spend the entire weekend guarding a prisoner that had a psychiatric emergency.
They had to assign two officers to guard the prisoner for a 48 hour period because of a delay in the psychiatric screening. Most of the time spent by the officers was on overtime. The cost was thousands of dollars from the police department budget.
Many Chiefs in attendance agreed they had experienced the same problem in the past and just one prolonged incident could strain an agency’s budget. During the meeting the Chiefs turned to Middlesex County Prosecutor Bruce Kaplan to help find a solution to this costly problem. Prosecutor Kaplan advised the County Chiefs he would discuss the issue with Middlesex County Jail Warden Edmund Chicci and see if a cost effective solution could be found.
At the next meeting Prosecutor Kaplan and Warden Chicci presented the idea of telepsychiatry. Telepsychiatry is a process that screens prisoners through a video conference. If the program could be implemented law enforcement agencies in Middlesex County would have the ability to have a prisoner with a psychiatric emergency examined by a psychiatric clinician 24 hours per day / 7 days a week / 365 days a year.
CFG Health Systems (sister company of Array), the current provider of medical services for the Middlesex County Jail, and numerous correctional facilities throughout New Jersey and Pennsylvania, was willing to work with the association and run a test pilot program for six months. A committee was formed consisting of law enforcement executives from the Middlesex County Chiefs of Police Association and county officials to study the possibility of implementing a telepsychiatry program.
All the law enforcement executives on the committee agreed that in order for the program to succeed it would be important to minimize the number of trips to local hospitals for the purpose of having a prisoner evaluated.
It is common knowledge among criminals in Middlesex County that you could avoid or delay entry into the county jail by claiming you are suicidal or you are experiencing psychological issues.
Often prisoners would threaten suicide so they could spend time in the hospital instead of the jail. These trips are costly and present security risks. If the trips could be minimized the officers would be available to patrol the streets and the cost to guard these prisoners would be greatly reduced. This was the main goal of the program.
The committee worked with County Jail officials to set up a procedure to have the prisoners screened. A prisoner experiencing a psychiatric emergency or threatening suicide that was set to be lodged in the county jail would be transported similar to a prisoner being lodged under normal conditions.
The only difference would be that the agency transporting the prisoner would be required to notify the jail prior to transport the need for a psychiatric screening. This would give the jail staff time to contact the on-call psychiatric technician and set up the video conference monitor. The officers transporting the prisoners would have to stay with the prisoner throughout the screening until the prisoner has been cleared for lodging at the county jail.
The psychiatric clinician could determine the prisoner is medically cleared to be lodged at the jail and recommend strategies to the jail staff to safely secure the prisoner. The clinician could also determine if the prisoner needed to be transported to a psychiatric hospital.
During the six month test period the average waiting time the police officer has had to spend with the prisoner during the screening was 65 minutes. The time saved transporting the prisoner and waiting for treatment was drastically reduced.
Dunellen Police Chief Gerard Cappella stated “in my 23 years of law enforcement I have never seen a psychiatric screening at a hospital conducted in less than six hours. The time saved is worth participating in the program.”
The main goal of the program was achieved immediately. The amount of time local law enforcement officers were guarding prisoners at hospitals for psychiatric emergencies is almost non-existent.
Police officers can return to the streets faster to perform their normal patrol functions.
It is estimated that in less than six months the savings in overtime expenditures was approximately $75,000. The cost of the program is divided among 26 law enforcement agencies in the county. Each agency is charged per capita based on the population they serve.
The program is considered by many law enforcement executives a great insurance policy. If you use it one time you can recoup your cost by not paying officers overtime to guard prisoners at local hospitals. The total cost for the program will be $36,000 per year.
Monroe Township Police Department was the first agency to use the program. Their cost to participate in the program is $1,383 per year.
The officers brought the prisoner to the county jail on a Friday night. After the prisoner was assessed by the psychiatric clinician she was approved for clearance at the jail. The clinician recommended that the jail conduct a suicide watch for 24 hours which they are equipped and trained to do.
Monroe Police Chief John Kraviec stated “if this situation occurred prior to the implementation of the program my officers would have been stuck at the hospital all weekend guarding the prisoner. It would have cost thousands of dollars in overtime. The program pays for itself the first time you utilize it. My officers came back and told everyone how smooth the system ran. It’s a benefit to the taxpayer by reducing cost and it makes your agency more effective.”
There have been other benefits for law enforcement since the program has been implemented. Officer morale has improved because they now know what to expect when they have a prisoner with psychiatric issues.
Prior to the program being implemented the police officer did not know if they would be stuck guarding the prisoner for an hour or days on end.
This has also led to a better relationship with the jail staff. It is very clear now what the role of the police officer is and at what point the prisoner will become the responsibility of the jail staff.
The prisoner is assessed much sooner and the liability for everyone is reduced because of the faster diagnosis and prescribed treatment. Middlesex County Freeholder Mildred Scott, chair of the county Law and Public Safety Committee, a 28 year veteran and retired Chief Sheriff’s Officer of the Middlesex County Sheriff’s Department recalls being tied up for hours in hospitals with prisoners. “This program improves officer safety and saves the taxpayers money.”
Middlesex County Deputy Freeholder Director Christopher Rafano, who was part of the committee and instrumental in implementing the telepsychiatry program, stated “there will be no reduction in treatment for the prisoner. In fact the treatment would be better because the prisoner will be evaluated faster than if brought to a hospital.”
Les Paschall, CEO of CFG Health Systems emphasized that the program is designed to comply with the Standards for Healthcare Services in Correctional Facilities issued by the National Commission Correctional Healthcare.
It is also designed to meet all constitutional and regulatory requirements as well as the local community standards of healthcare. This innovative solution is an example of a shared service that has proven efficient and effective which is imperative
in these difficult economic times.
Prisoners with psychiatric emergencies are treated expeditiously reducing liability to the arresting agency. More importantly police officers are spending less time at health care facilities guarding prisoners and are available to protect and serve the residents of Middlesex County.
Ray Hayducka is Chief of Police in South Brunswick Township. He currently serves as the 3rd Vice President of the NJ State Association of Chiefs of Police.
Many Americans in rural areas struggle to access high-quality mental health services due to a chronic shortage of providers, costs and time associated with care, and persistent stigmas surrounding seeing a behavioral health specialist. As the growing opioid crisis and other factors create a higher demand for care, this lack of access becomes even more urgent. That was the case at OSF HealthCare’s Saint Elizabeth Medical Center in rural Ottawa, Illinois, which faced an influx of patients with untreated mental health and substance use disorders.
Due to the compounding issues of provider shortages and rising demand, patients were at risk of subsequent psychiatric hospitalizations while OSF faced potential decompensation. Wait times for in-person psychiatric care and for services at the CHOICES outpatient department had ballooned to six months. In addition, some patients were reluctant to visit a psychiatrist because of stigmas surrounding mental illness, costs associated with treatment, and time required to travel to appointments away from their primary care facility, all impeding the ability to receive the care they needed.
Recognizing its challenges and facing the reality of long patient wait times, OSF aimed to erase barriers to care at Saint Elizabeth Medical Center through an innovative approach to these issues.
In 2017, OSF launched a telepsychiatry program featuring direct-to-patient care as well as eConsult services. To bring its telehealth and eConsult programs to life, OSF turned to Array Behavioral Care, a leading provider of integrated telepsychiatry services. Array's eConsults empower primary care providers to treat some issues themselves, ensuring mental health clinicians are available to treat more severe conditions.
“Array has been a tremendous partner to our organization as we roll out an array of telepsychiatry options, including innovative consultative and patient treatment approaches,” says Luke Raymond, manager of behavioral health at OSF HealthCare. “Array demonstrates a commitment to customer service, high-quality psychiatric care and effective communication.”
Before referring a patient for direct psychiatric care, OSF’s primary care providers leverage eConsults to contact a Array clinician and determine if a referral is clinically appropriate. Based on the telepsychiatrist’s responses, a primary care provider may prescribe medications directly to the patient or refer them for additional services as needed. Providers also use eConsults to help patients access treatment more quickly when appointment wait times are significant.
eConsults are helping to decrease psychiatric wait times by enhancing the capacity of primary care physicians to provide mental health services. In addition, eConsults can increase the likelihood of patients seeing a mental health clinician, since they can more easily navigate the social stigma of seeking treatment and are often more comfortable talking to their primary care providers. For patients who still need to see a behavioral health specialist, Array clinicians provide telepsychiatry services through the secure ArrayConnect™ platform.
Through its partnership with Array, OSF is significantly expanding access to care while ensuring each patient receives the right level of services. The telehealth and eConsult programs have helped OSF:
Reduce patient wait times dramatically. By adding Array telehealth clinicians for direct-to-patient care and reducing unnecessary referrals through eConsults, OSF has slashed patient wait times from six months for in-person consultations to six weeks for telepsychiatry sessions, a 75 percent reduction in wait In total, Array has completed more than 1,000 direct patient sessions and provides about 25 eConsults monthly.
Deliver patient and provider satisfaction. More than 98 percent of telepsych patients give the experience high marks. Among OSF providers surveyed about the eConsult program, 88 percent are satisfied with the content and 91 percent are satisfied with Array's response times.
Drive continuous improvement. The HIPAA-compliant ArrayConnect platform, designed specifically for telepsychiatry, securely and effectively connects patients with Array clinicians while offering session data and reporting tools so OSF can monitor program success. Array's deep pool of clinicians also gives OSF the flexibility to grow, with the two organizations already discussing expanding the program to new sites.
Based in southern Oregon, Cow Creek Health and Wellness Center operates two clinics that provide a full suite of healthcare services to the Umpqua tribe and surrounding community. Like many Native American communities, however, Cow Creek found itself with a significant need for mental health professionals – and no effective way to meet the needs of its members.
The need was particularly prevalent among county residents and patients of the center who struggle with a variety of behavioral health issues, including post-traumatic stress disorder, alcohol abuse, depression, anxiety and suicide. Additionally, Cow Creek was unable to locate a child psychiatrist for either of its clinics, resulting in patients either going without treatment or traveling anywhere from 60 to 120 miles for child psychiatric care.
Clinical staff viewed the gap in treatment as unsafe and harmful to the community. They knew they needed a clinician, but the recruitment process was difficult and expensive. There were few board-certified child psychiatrists in the region, and Cow Creek would need to find someone who could meet both the clinical and cultural needs of its patient population. The clinic saw telepsychiatry as a way to access a much larger pool of quality clinicians who could serve its patients, regardless of location.
Being new to telemedicine, Cow Creek looked to Regroup, a leading provider of integrated telemental health services, to match a clinician and meet their mental healthcare needs. With deep behavioral health expertise and a large clinician network, Regroup focuses on finding the right clinician while providing comprehensive support, from program set-up and launch to ongoing assistance at every level.
These all-inclusive elements ensure the best possible outcomes for patients and staff alike.
For Cow Creek, the right clinician was someone who would be culturally sensitive to the challenges that tribal populations face, including intergenerational and historical trauma. Beyond that, they were looking for someone who could get along well with on-site staff members and be “focused on patient care, not ego,” clinic director Dennis Eberhardt says. Regroup matched the clinic with a seasoned child and adolescent psychiatrist with extensive experience treating family trauma and anger management, two areas of focus for Cow Creek patients. The Regroup clinician has been well-received by staff and patients alike, putting patients of all ages at ease while quickly adapting to Cow Creek’s workflows and collaborating with on-site staff to provide seamless, holistic patient care.
In fact, the psychiatrist proved so successful that patient demand quickly exceeded the clinician’s weekly hours. Working with Regroup, Cow Creek was able to expand its services easily to see more patients each week. Cow Creek also turned to Regroup for non-prescribing needs after losing two of its on-site therapists. Regroup provided a licensed clinical social worker (LCSW) to serve Cow Creek’s adult population, who has also proven to be an excellent fit. Though many adult patients were initially hesitant about what to expect with an on-screen therapist, the Regroup clinician’s warm and welcoming personality won them over, so much so that the clinic is now looking at expanding her hours as well.
Through its partnership with Regroup, Cow Creek is able to provide exceptional mental healthcare to all its patients, including children and adolescents. Key benefits include:
Convenient access to quality care. With instant on-screen access to experienced, caring clinicians, the entire Cow Creek community is finally getting the mental health support it needs. Children and their families no longer have to travel hours to see a quality child psychiatrist or wait weeks to see a therapist, and feedback from patients has been overwhelmingly positive.
Flexible, affordable resources. While Cow Creek initially began its telepsychiatry program with a single child and adolescent psychiatrist for a few hours a week, the clinic was able to easily expand his time as demand Similarly, as demand for a therapist has grown, the clinic has been able to seamlessly increase its LCSW’s weekly hours. According to Eberhardt, being able to right-size services and only pay for the hours needed is “one of the beauties of telepsychiatry. The flexibility and the ability to scale incrementally like that are very valuable.”
Wraparound support. As it launched telepsychiatry for the first time, Cow Creek found it invaluable to have a partner to guide the organization through every step of the implementation process. Post-launch, Cow Creek knows that Regroup is there to provide support for every aspect of the program, from technical questions to regulatory updates. Although a Regroup Account Manager regularly connects with the team at Cow Creek to see how they’re doing, Eberhardt has continued to report “smooth sailing.”
Success breeds success. As word of the success of its telepsych program has spread, Cow Creek has begun attracting additional mental healthcare providers. One local psychiatrist reached out based on the program’s reputation and plans to join the on-site staff soon. “Earning that type of reputation means lowered recruiting costs, as well as ensuring a top-notch team of clinicians,” Eberhardt says.
 As administrators of a general hospital with no specialized psychiatric unit, leaders at Chester County Hospital in eastern Pennsylvania had become accustomed to a waiting game for psychiatric consultation when a patient with clear mental health needs presented in their emergency department. As is the case at a growing number of general hospitals around the country, telepsychiatry is providing these leaders with an alternative to what can become a crisis in emergency operations — as well as for patients in need.
As administrators of a general hospital with no specialized psychiatric unit, leaders at Chester County Hospital in eastern Pennsylvania had become accustomed to a waiting game for psychiatric consultation when a patient with clear mental health needs presented in their emergency department. As is the case at a growing number of general hospitals around the country, telepsychiatry is providing these leaders with an alternative to what can become a crisis in emergency operations — as well as for patients in need.
In partnership with national telepsychiatry company InSight Telepsychiatry, LLC, Chester County Hospital is now using video technology to enable it to receive expert consultation on cases, usually within an hour of making initial contact.
This reduces wait times for services and creates more effective referral to specialty mental health treatment services in the community, while in other cases it simply might offer a more rapid and expert confirmation that a patient with mental health needs can be safely discharged.
“In the emergency department, the availability of specialty services is always difficult,” Betty Brennan, Chester County Hospital’s director of emergency services, told MHW.
“We were finding that the availability of psychiatrists was increasingly more difficult, because of their professional load in their offices. The immediacy that we needed just wasn’t there.”
The hospital’s phone calls to other facilities to see how they were handling the issue of delays in mental health patient transfer or discharge led the organization to InSight in 2011.
Brennan said the high quality of communication between patient and remote provider via video gives her confidence that the sessions between patient and psychiatrist virtually duplicate the more common face-to-face experience. “You almost forget in today’s world that you’re talking on videoconference,” Brennan said of the telepsychiatry experience.
The hospital launched its work with telepsychiatry for evening and overnight hours but has since expanded the program in order to maintain round-the-clock coverage.
In a typical scenario, a patient might present with suicidal ideation and be seen immediately by an emergency physician on the hospital staff. Once an initial level-of-care evaluation takes place in the ER setting, the hospital will contact In- Sight’s Access Center and transmit a patient history.
Brennan said InSight provides a number of psychiatrists for the telepsychiatry services, and the hospital has been able to develop a rapport with these individuals over the course of the project. (The psychiatrists are required to be credentialed at the hospital facility with which they are working.)
Often the hospital staff physician will speak with the psychiatrist before the specialist conducts the patient interview. For the video interviews, the hospital uses several secure rooms that are located a fair distance from any hospital exits. A hospital employee, such as a nurse or a member of the security team, is required to be present while the patient is being assessed via video.
The interviews are highly detailed and usually last anywhere from 20 to 45 minutes, Brennan said.
The high-definition videoconferencing equipment helps to establish a process that very closely approximates what occurs in a face-to-face interview, she said.
“We’ve never had a patient refuse,” Brennan said, as the message to them becomes one of facilitating necessary services in the quickest manner possible. “The physicians are very skilled, and the patients like that it’s private.”
A written consult from the psychiatrist is faxed to the hospital upon completion of the specialist’s interview and evaluation. “We’re not waiting for a psychiatrist to come in when his office hours are over,” Brennan said.
Often it is the case that the psychiatrist’s consultation offers a rapid confirmation of a course of action that was already apparent to the hospital staff, from a referral to a specialty behavioral health facility in the community to a discharge without extensive follow-up.
Brennan added that having this service available not only helps establish more effective linkages with mental health providers outside the hospital for followup care, but also speaks to a more humane way of addressing patient needs.
“There is an increased focus now on the rights of the mental health patient, and on getting them to the right facility,” she said.
Brennan believes the telepsychiatry option can work equally well for adult and adolescent patients. The secretary of the Delaware Department of Health recently said that telepsychiatry could assist in reaching underserved young people in a state that this year has seen a significant number of teen suicides related to unaddressed mental health needs.
Brennan said the telepsychiatry experience at Chester County Hospital has proven so effective that the hospital has begun to extend telehealth into other operations. It is now using similar technology for evaluations of stroke patients, she said.
Other hospitals across the country that are working with InSight technology have reported similar improvements in wait times and overall emergency operations as a result of telepsychiatry’s availability.
“On occasion, patients are taken to the hospital under the Baker Act for a behavioral issue when they’re actually under the influence of drugs or alcohol,” said Eddie Carie, behavioral health case manager at South Florida Baptist Hospital in Tampa.
“These patients used to wait days for a psychiatrist’s evaluation. Now, we’re able to have a psychiatrist evaluate the patient and make a decision within hours.”
Inspira Health Network, a nonprofit, three-hospital health system serving communities across southern New Jersey, lacked psychiatric providers, resulting in delays in service. Consults have a 24-hour window, which led to bed, intervention and recommendation delays for medical patients.
As a result, it was not unusual for patients to wait longer than 24 hours for psychiatric consults due to a lack of available psychiatrists. Because many patients were accessing services through the emergency department, this protracted wait period created bottlenecks and bed delays. In addition, needed psychiatric interventions and medication therapies were delayed that could help stabilize patient conditions as emergency department staff waited on the direction of specialists with the right expertise.
Inspira Health Network chose to work with the Center for Family Guidance and its sister company, InSight Telepsychiatry, a national service provider that aims to improve access to behavioral healthcare through telehealth technology.
“We opted to use telepsychiatry for psychiatric consultation of medical inpatients to promote efficiency, access and throughput,” said Sarah Seabrook-DeJong, RN, director of psychiatry services at Inspira Health Network. “The expectation was that around-the-clock, real-time access to psychiatric resources would improve patient throughput and speed care delivery processes.”
Patients would receive needed interventions quicker, resulting in better outcomes and higher levels of satisfaction, she explained. The new technology-enabled process would also create workflow efficiencies and lend to less bottleneck in the emergency department, ultimately improving the hospitals’ bottom line, she added.
In addition, around-the-clock access to psychiatric consults would improve provider satisfaction as patients would receive high quality, “whole person” care in a timely manner, said Seabrook DeJong.
“This would allow for 24/7 access to a psychiatrist through a remote video conferencing model, which would promote interventions, recommendations and dispositions to transpire much more quickly and effectively,” she explained.
There are many vendors on the market today offering telemedicine technology, including American Well, Avizia, GlobalMed, MDLive, Novotalk, SnapMD, Teladoc, TeleHealth Services, Tellus and Tyto Care.
Inspira Health provided iPads on mobile carts and a Bluetooth speaker that go directly to a patient’s bedside for a consultation. This new workflow was designed to address inpatient admissions going to the medical floors at two of Inspira’s hospitals. While the system does not currently offer inpatient psychiatric services, some patients require psychiatric consultation prior to leaving the emergency department.
“The telepsychiatry iPad is managed by the nursing supervisor, who deploys the cart when requested,” said Seabrook-de Jong. “The consultation with the patient is monitored by either a medical technician or nurse to ensure patient safety while not affecting confidentiality.”
“By creating a clear, efficient process, modeled after an existing one for teleneurology, staff were educated on the flow and steps to accomplish a consistent experience and expectation for patients.”
Sarah Seabrook-DeJong, RN, Inspira Health Network
The telepsychiatry system is a separate, HIPAA-compliant app with the telepsychiatrists documenting directly into Inspira’s EHR. The telepsychiatry service is integrated with Inspira’s Cerner EHR. InSight’s telepsychiatrists document into Cerner, improving workflow efficiencies and allowing information to be shared in near-real time, she said.
“By creating a clear, efficient process, modeled after an existing one for teleneurology, staff were educated on the flow and steps to accomplish a consistent experience and expectation for patients,” she explained. “Having a designated liaison between Inspira Health Network and InSight telepsychiatry was critical to the success of the innovative technology and new process.”
Inspira Health has seen response times around two hours from request of consult to completion of the assessment. It is able to secure a disposition from a specialist, enabling the hospital attendings to determine treatment care directives, consideration of psychiatric admission, discharge, initiation of effective psychotropics, and more.
“Nearly 100 percent of behavioral health consults are now completed through the telepsychiatry provider,” said Seabrook-de Jong. “Only in rare cases are alternative options employed. For instance, a face-to-face consult was ordered for a deaf patient who used a hearing device. This new technology-enabled approach to care processes has allowed us to substantially reduce wait times and improve throughput.”
Notably, pushback from medical staff has been minimal, she added.
“Hospital physicians appreciate having near-real-time access to psychiatric consult information and the fact that patients receive interventions in a timelier fashion,” she said. “The fact that all staff are agreeable to this change speaks to the initiative’s success.”
This model was so successful in its initial implementations that Inspira Health Network has selected it for their newest hospital, to open in November 2019, as it fits the future needs and use of technology perfectly, she said.
